Ask many EMS CQI professionals how they CQI stroke calls and you are likely to hear their efforts revolve around recognition, treatment, and stroke alert notifications. Certainly, that is a good place to start. But as with all CQI efforts, simply collecting data points to produce reports and statistics can lead to misleading corrective efforts.
To make a real impact on improving outcomes for stroke patients, CQI officers need to understand the issues that providers oftentimes miss and why, to bridge the gap between good versus not-so-good patient care.
There are many elements of a stroke type call that providers are expected to know and act upon to ensure this patient population is properly cared for.
The most common reason for stroke patient errors is simply missing stroke as a potential differential in diagnosing the patient. This error will not show up in your stroke dataset if you are using the standard reports from your ePCR as the report cannot identify when a stroke patient was simply misdiagnosed. As a result, using those reports to determine if your agency’s care is adequate for this patient group is likely to mislead you and provide a false sense of confidence.
It is quite common for providers to miss CVA as a cause of illness, especially for the atypical stroke presentation. If the patient is having a complaint of visual disturbances as their chief complaint, the provider may not think of assessing the patient fully for CVA by doing a stroke exam for example. Without that formal exam, it cannot be fully determined if this patient met the criteria for stroke care and a stroke alert.
Another big miss by providers occurs when the provider accepts the patient’s opinion of what is wrong with them instead of verifying what they think is wrong with the patient based on an objective, full exam. We see this often when a patient states their symptoms are consistent with the patient’s history of (fill in the blank here), and they believe that is what is wrong with them today. The field provider accepts this rationale and goes with it as opposed to doing a full exam and determining for themselves that this is the likely cause of the patient’s current complaint or condition.
In stroke patients, this may sound something like the patient stating they are having a very bad headache, but they have a history of migraines, and they believe this is just a bad migraine episode. It may be, or it may be a sign of a CVA. Without the provider providing independent verification through a full exam and more in-depth questioning, a diagnosis of stroke may be missed.
Data should be collected on a variety of potential improvement items that may not show up on a standard CVA report. The G&A Stroke Summary Report (see report below) lists many of the common data points we collect, but we also screen for a variety of other common errors. You may also want to collect data on other common issues providers miss including:
- Documentation of anticoagulant use
- Proper O2 therapy for this patient population (maintaining a sat between 94-99%)
- Scene time delays
- Blood glucose and 12 lead acquisition
- The documentation of both a full neuro exam and a formal stroke exam (many providers don’t fully understand the difference between the two and think a good neuro exam is good enough in determining whether a patient is having a stroke)
- A detailed last know well time and symptom discovery time (providers often provide general times like “last night”, or “this morning” as opposed to a specific time estimate)
- Documentation on how the patient was moved showing that the patient was not allowed to exert themselves during the movement process (we often see stroke patients allowed to walk to the stretcher or in some cases, out to the ambulance for example)
- Lack of stroke alert to receiving facility
Providers sometimes do not provide a stroke alert when they are not certain the patient is having a stroke. Even though the patient meets the protocol criteria for a notification, they are sometimes reluctant as they do not want to be wrong and call a non-stroke a stroke. Understanding when to call the alert is critical to getting compliance and eliminating the doubt about when to activate the stroke team.
It is a good idea to discuss with the provider how best to handle cases where they are either not sure, or not convinced that a stroke alert should be given. Online medical control can help if there is indecision or providers can also have a discussion with the person accepting the entry notification at the receiving facility that they are required to give an alert but the patients presentation in not likely CVA even though they meet the criteria.
Discussing the patient’s clinical presentation may clear up whether the receiving facility wants to activate or not. The provider should document that they gave an alert as required but after the patient report was given the hospital staff decided they did not feel this patient would benefit from a stroke activation.
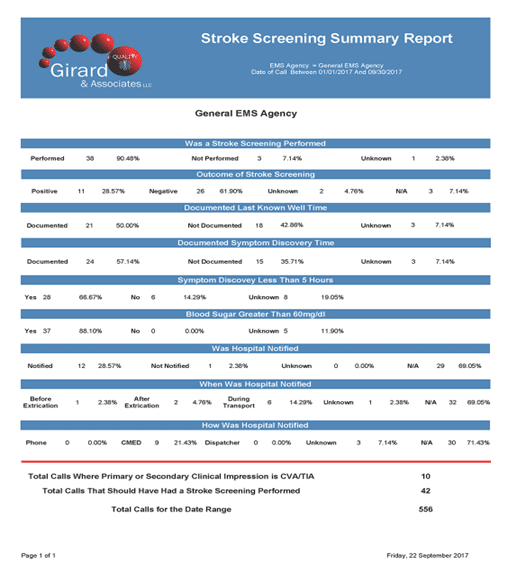
As you can see from this report, providers at this agency had a total of 10 calls where they determined the primary or secondary clinical impression was CVA. However, there were a total of 42 calls where the patient had a complaint or presentation that should have triggered a stroke exam to help determine if the patient was actually having a stroke.
Of the 42 patients who should have had a stroke exam, 38 received one (very good), but 3 patients did not and on 1 patient it was not clear from the PCR if the patient was fully assessed to make that determination. That means either 3 or 4 patients (between 7.14% and 9.52%) may have been missed for possible stroke due to a lack of a full stroke exam. These calls are often overlooked in many stroke data reports.
There are many opportunities to improve stroke care beyond the standard basic metrics of traditional stroke data. There is much more to ensuring these patients are well served than a simple numerator and denominator in a stroke report. Be sure to understand and collect data on ALL the common provider errors that can occur.
For more information on this topic check out our podcast on CQI’ing the stroke patient, CQI And the Stroke Patient: What Could Possible Go Wrong?
Or you can go to www.girardassoc.com for more information.
For more topics like this check out our other EMS CQI articles:
Preventing the Provider Induced Patient Refusal (PIPRs)
Timely Topics in EMS CQI: The ACS patient
Do I Really Need to Document How I Moved My Patient?
Timely Topics in EMS CQI: The ALS Downgrade Note
You can contact the author at, paul.girard@girardassoc.com