Ever try to calculate the return on investment of your EMS CQI program? Pretty tough, right? After all, performing QA/QI/CQI functions is intangible and difficult to quantify, especially in financial terms. Not to mention that in strict accounting terms your return on investment is normally a function of how much net return (gross revenue – expenses) you receive in return for capital expended. For most EMS agencies, the CQI function is a strict expense center with no revenue attached, so you are not getting too much financially for your CQI efforts.
Unfortunately, as many agencies regard CQI efforts to be an expenditure without much return, they tend to under capitalize the QI department. This oftentimes results in a poor CQI program that is ineffective in obtaining results (demonstrable improvement in patient care/protocol compliance) and creates resentments on the part of field providers, as the process appears to be unevenly applied and just outright error prone!
Is it even possible to create an analysis of the CQI process that can produce measurable results? You bet it is! There are three primary categories that can be measured and quantified that can provide a high level of confidence that your CQI dollars are well spent.
- Measuring patient care performance
- Measuring provider satisfaction
- Measuring potential increased revenue from your CQI efforts
Measuring Patient Care Performance
There are many ways to measure performance in EMS systems, but most measurement tools do not look at the agency or providers total body of work in a measurable way.
Simply put, there are few tools out there to do so. Instead, EMS systems generally measure specific criteria such as response times, STEMI recognition rates, cardiac arrest outcomes, or statistical skill categories such as IV or intubation success rates. While all that data is helpful, it doesn’t really show performance in a complete manner. An agency or provider can have difficulty in one area and be exceptional in another, but the provider will usually only hear about their problem areas come QA review time.
Much of the data that is used in EMS are reports that come out of the services ePCR program, but such programs are highly inaccurate in the data supplied, as much of the data has not been vetted first. Take STEMI recognition rates as an example. If you are using the reports from your ePCR program, you may have a problem. The reports are generated from the data that is put into the system by the providers themselves and are prone to inaccuracies, bias, and sometime outright manipulation.
The STEMI report will only give you data when the provider has flagged the call as a possible STEMI, but what about the 80-year-old little old lady who has had general weakness for 4 days that the medics did not think to do a 12 lead on. How do you catch and measure that data? QA personnel would need to read every report and 12 lead EKG to find the calls where a 12 lead was not performed that should have been, as well as review every 12 lead that was performed to ensure that a STEMI was not missed.
For smaller agencies that do 100% QA reviews this may be feasible, but for larger agencies that do sampling there are many calls that may be missed. Providers know this reality. That is why they get frustrated with the CQI process. All that data needs to be aggregated to show overall performance and not just a variety of individualized stats. In our system, we use a scoring matrix for every call audited that uses a risk index to quantify any potential risk to the patient, thereby allowing us to provide a numeric value. Besides the individual data there is a performance rating.
Every provider in the agency gets a personalized report with the data noted above and every call is reviewed with the provider, so nothing is overlooked. As every provider is given the same data and goes through the same review process, there are no claims of bias or selective enforcement of regulations/protocols.
Measuring Provider Satisfaction
Does you CQI process create a lot of stress and drama? Do providers feel they are not getting a fair assessment? Perhaps you should measure the satisfaction of your providers with the CQI process. This can be achieved in a variety of ways but getting good feedback from your staff members on how they think the process is working and what can be improved on in the improvement process can go a long way in building trust in the process. Trust in the process usually results in increased compliance and cooperation. While some people will never actually like the CQI process, you can do a lot to reduce the friction between the CQI staff and the field providers. Simple questionnaires and feedback forms can be used and structured in a manner that allows for easy understanding as to whether your CQI process is successfully reaching people.
In most dysfunctional QA/QI systems we see, the most often complaint is that the process is accusatory and punitive. The solution is creating an education-based QA/QI feedback process that promotes teaching, coaching, and mentoring, and less criticizing. If providers feel the process is there to help them be better providers, the likelihood of buy-in is much greater. Reduce the friction, improve the results!
Measuring Potential Increased Revenue from Your CQI Program
So, you do step 1 and step 2, but do you ever try to quantify the potential return in dollars and cents? Admittedly, this one can be a bit tricky but there are a couple of areas that may be useful in measuring the dollars lost (or captured) that can be direct result of your CQI efforts.
Pretty much every agency we work with has been able to capture lost revenue once the CQI process gets established. The money recaptured can be sizable and may help to fund your CQI efforts. To listen to our Podcast on EMS CQI Return on Investment, Click Here!
Opportunity 1 – Patient refusals
In many of the agencies we provide services for, one of the easiest areas we find lost revenue is in the patient refusal process. Most agency managers realize that patient refusals are high risk for litigation, but it can also be a drain on your cash flow. In services where the patient refusal process is not well monitored, it is not uncommon for providers to obtain refusals on patients who really should be transported.
While patients have the right to refuse EMS care, oftentimes providers actively solicit refusals either explicitly “(you don’t need to go to a hospital”), or implicitly (“the ED is very busy right now and you may have to wait a long time to be seen”). When providers become aware that every refusal they write will be reviewed for appropriateness as well as proper documentation they become less likely in trying to obtain a refusal and will often make a more concerted effort to convince the patient who needs to go to the hospital that they need to go. A refusal now becomes a transport that can be properly billed. On some level pretty much every agency we start with has an issue with this. Most agencies see between a 5% and 35% reduction in refusals (into transports).
One agency reported they saw a conversion of refusals to transports that resulted in recouped revenue of $75,000 per year annually. That recapture not only covered the cost of hiring us to perform their CQI functions, but also added to their bottom line by a sizable amount. Not only did they collect the missed revenue but their Performance score rating improved for the calls that remained refusals. In other words, the refusals they did execute became more defensible and properly documented which decreased their liability exposure. Talk about a win-win!
Opportunity 2 – BLS’ing ALS calls
Another opportunity for increasing revenue through proper CQI efforts is in the BLS to ALS conversion. This is especially true for agencies that do sampling and do not audit a large portion of their BLS calls. The thinking is that the BLS calls are less risky from a medical-legal perspective and the CQI efforts can be better spent looking at the critical patients or high-risk categories. Every single agency we have encountered that has that thought process came to find that they were missing a fair amount of patient care encounters whereby the patients did not receive ALS care that should have.
In some instances, ALS providers do not always provide ALS services to patients who needed such care. It may be due to not recognizing the potential seriousness of the patient’s condition or may be due to just not wanting to put that level of effort into their job (that’s the polite way of saying laziness). If a lazy provider knows that the agencies CQI process does not spend a lot of time looking at BLS calls, that is an added incentive to BLS the call. Not only do they not have to do the work, but the call is less likely to be reviewed by the QA/QI process. That is a win-win, for the provider! It is a lose-lose for the agency.
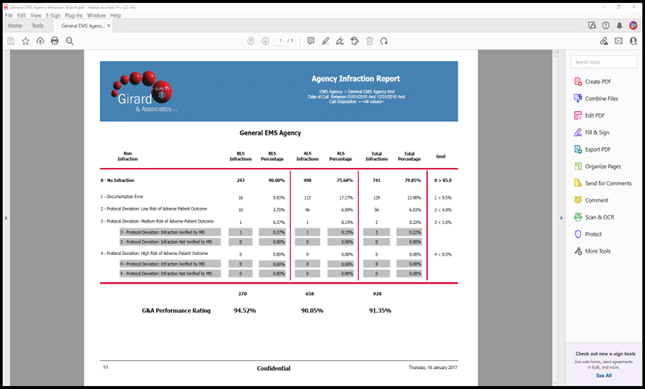
The risk of patient harm is much greater (as is the potential for litigation) and the revenue loss can be substantial. Especially if the agency culture is pervasive in this regard. The agency in the example above regarding the patient refusal issue also had a triage to BLS problem. It turned out that 178 calls per year were being BLS’d that should have had ALS. The financial implications for this issue resulted in another $54,000 per year in revenue. The return on investment for this agency looked like the chart below. You can download an Excel Spreadsheet here to enter your own numbers to find your potential revenue recapture.
| Cost of Outsourcing CQI Program (specific to the agency discussed in this article) |
$46,000 | |
| Recaptured Revenue | % Return | |
| Patient Refusals | $75,000 | |
| Missed ALS Opportunities | $54,000 | |
| Total Recapture (Gross ROI) | $129,000 | 180.43% |
| Return On Investment (Net ROI) | $83,000 | 80.43% |
Opportunity 3 – ALS level 1 calls that should be ALS level 2, Canceled On Arrival/Enroute
There are other revenue recapture opportunities as well. Through poor documentation or treatment, calls that may be billable at an ALS level 2 may only get billed at the ALS level 1, thereby decreasing revenues. For agencies that bundle bill for intercept services, there may be instances where providers are not even writing a run report, and labeling a call as canceled on arrival (or enroute) by the BLS service on scene when they in fact arrived on scene. This may result in a different version of a call that should have been ALS’d but was let go BLS to the mutual aid agency. This not only results in lost revenue and increased risk but damages the ALS intercept service’s reputation with their mutual aid agencies.
Opportunity 4 – Insurance Premium Reductions
Another consideration is any insurance premium offsets. On occasion, agencies we work with have mentioned that their insurer gave them a reduction in premiums for having a third-party QA service. The reports we produce for management on a trimester bases are shared with the insurer so they can see the improvement trimester to trimester. They saved 10% off their liability premiums. It is worth asking your insurer if there are any saving to be had and adding any savings to your calculations when determining your ROI for your service.
Conclusion
Many EMS agencies tend to under fund their CQI initiatives with the outdated thinking that CQI efforts are a loss leader. Something you need to do, but it drains the services financial resources. The reality in many cases is that an underfunded CQI program cannot do the job it is designed to do. This may result in not only not improving the service’s patient care but increasing risk to the service and in many cases, results in lost revenue that could be captured if the CQI personnel had the resources to do the job properly.
You may even find that the increase in revenue exceeds the cost of funding the CQI program. An analysis of the benefits of a properly funded CQI program should be carefully examined to understand to true cost of providing this critical service. Check out our ROI calculator where you can enter your own numbers to show a potential increase in revenue by outsourcing CQI.
For more information visit us at www.girardassoc.com or contact Paul Girard at paul.girard@girardassoc.com.